Newswise — Jan. 15, 2025 - Women who were cared for by the MedStar Health D.C. Safe Babies Safe Moms program (SBSM) have better outcomes in pregnancy, delivery, and postpartum, according to a . Additionally, the study showed that Black patients cared for by SBSM were also less likely to have low or very low birthweight babies or preterm birth than Black or White patients who received prenatal care elsewhere.
The U.S. faces some of the highest maternal and infant mortality rates among developed countries, with significant racial and geographical disparities. In fact, Black birthing individuals are at a considerably higher risk of adverse maternal health outcomes compared to their White counterparts, even when factors such as education and employment are comparable.
"We know that maternal health has for too long been a dark spot in the American healthcare system. And while there are many contributing factors, a major cause of these disparities is structural and systemic racism," said Angela D. Thomas, DrPH , executive lead for SBSM and first author for the paper. "With Safe Babies Safe Moms, we have strived to build a program that addresses equity at the root while aiming to create an example that other health systems can replicate."
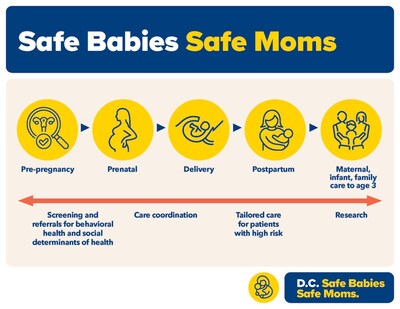
The SBSM program launched in April 2020 through a partnership with MedStar Health, the area's largest healthcare provider, and trusted community-based organizations, and . Together they have developed a model of care based on research and real-life experiences for birthing individuals and their babies from pre-conception, pregnancy, delivery, and the postpartum period through the first three years of life. SBSM has made considerable advances in improving outcomes in maternal and infant health. Other notable outcomes highlighted in the NEJM Catalyst paper include:
- Patients cared for by Safe Babies Safe Moms were 1.16 times less likely to have low birthweight babies, 1.40 times less likely to have very low birthweight babies, and 1.15 times less likely to have babies born preterm, compared to patients who received prenatal care elsewhere.
- SBSM prevented more than 58 preterm births in 2022, including 40 fewer preterm births among Medicaid insured patients and 18 fewer preterm births among privately insured patients.
- After adjusting for medical cost inflation at 4% per year, SBSM saved an estimated $5.16 million in medical costs associated with preterm births, or $89,000 per preterm birth prevented.
- Nearly all patients who screened positively for risk were referred to additional supportive services including tobacco cessation counseling (97%), breastfeeding education (96%), developmental milestones for infants/toddlers (95%), and social determinants of health referrals for families and postpartum patients (94%).
- All of the birthing individuals who screened positively for depression and anxiety were provided with mental health care (100%).
Using a newly developed framework that focuses on feasibility, sustainability, and equity, the care delivery model includes a suite of more than 70 interventions across six categories:
- Trauma-informed obstetrics and midwifery care
- Quality management and prevention of high-risk conditions that may complicate pregnancy or early childhood.
- Interprofessional care coordination between women and infants' services, pediatrics, family medicine, behavioral health, and community health centers.
- Universal screening for behavioral health (e.g., depression, anxiety) and social determinants of health for patients at key points during prenatal and postpartum care
- Integrated support services for patients at risk including services for housing, food insecurity, transportation, lactation and nutritional counseling, and pro-bono civil legal services.
- Health system and health IT innovations to enhance clinical and community transitions
"Safe Babies Safe Moms exemplifies the power of partnership in action," said Kelly Sweeney McShane, president and chief executive officer of Community of Hope and co-author of the paper. "We've created a program that truly transforms outcomes for birthing individuals and their families. Together, we're proving that equitable, comprehensive care is not just a goal but an achievable reality—one that addresses systemic disparities and creates lasting impact for the communities we serve."
Underpinning SBSM's integrated clinical and supportive services and community partnerships are research efforts from MedStar Health Research Institute to evaluate and further identify opportunities to improve maternal and infant care through further interventions. Additionally, researchers Carol B. Davis, PhD, assistant research professor and associate director of the Health Care Financing Initiative research center at Georgetown University's McCourt School of Public Policy, and Thomas DeLeire, PhD, distinguished professor and interim dean of the McCourt School, worked with the SBSM team to identify opportunities for novel payment models, strategies for additional cost-savings, and healthcare policies.
Over the next several years, MedStar Health hopes to scale the program to all of its hospitals that offer maternity care and serve as a national resource for other health systems looking to implement similar initiatives.
"As a learning health system, we use research to uncover new solutions about the best way to care for our patients. SBSM is a shining example of how innovative partnerships, evidence-based design, and commitment to advancing equity can make meaningful change for the most vulnerable patients and our communities," said Stephen R. T. Evans, MD, chief medical officer, MedStar Health. "We are excited about the next chapter for Safe Babies Safe Moms and being able to contribute to a solution to one of medicine's most pressing challenges."
Other authors of the paper include: Aza Nedhari, DHA, executive director and co-founder of Mamatoto Village; Loral Patchen, PhD, CNM, scientific director for SBSM; Matthew Biel, MD, chief of Child and Adolescent Psychiatry, MedStar Georgetown University Hospital and vice chair for Psychiatry, Georgetown University School of Medicine; Janine Rethy, MD, division chief, Community Pediatrics, MedStar Georgetown University Hospital and associate professor of pediatrics at Georgetown University School of Medicine; and Michelle Roett, MD, chair of Family Medicine for MedStar Georgetown University Hospital and Georgetown University School of Medicine.
The MedStar Health team's work was funded through an investment made by the A. James & Alice B. Clark Foundation to establish the initiative. For more information about the program and to learn more about ways to support it, visit .

